Table of Contents
Meet Cheelim Liew (BN, GradDipCriticalCare, MPH, GradDipCardiacUltrasound, CCRN | AMS, ECMO Advance Practice Nurse).
We are fortunate enough to have teamed up with Eastern Health to bring you this interview about the fascinating and intense world of an ECMO nurse (extracorporeal membrane oxygenation).
Introduction
I started my nursing career in 2002 after 2 ½ years of mandatory national service (Army). I came to Melbourne in 2005 to complete my critical care training and stayed in the Intensive Care setting since. There is only a handful of countries that have mandatory national service. If you have guessed correctly, yes I am from Singapore.
Intensive care nursing offers a variety of specialities. It ranges from trauma, and neurosurgery to cardiothoracic, transplant and Extracorporeal Life Support (ECLS) etc. My interests lie predominately in ECLS and cardiac ultrasound. ECLS includes Intra-Aortic Balloon Pump (IABP), Ventricular Assist Devices (VAD) and Extracorporeal Membrane Oxygenation (ECMO).
What is ECMO?
ECMO – heart/lung bypass machine (it’s layman term) is used to support patients who had suffered a reversible cardiac or lung failure that had failed conventional treatment. There are 2 major types of ECMO- VA (Veno-Arterial) and VV (Veno-venous) ECMO.
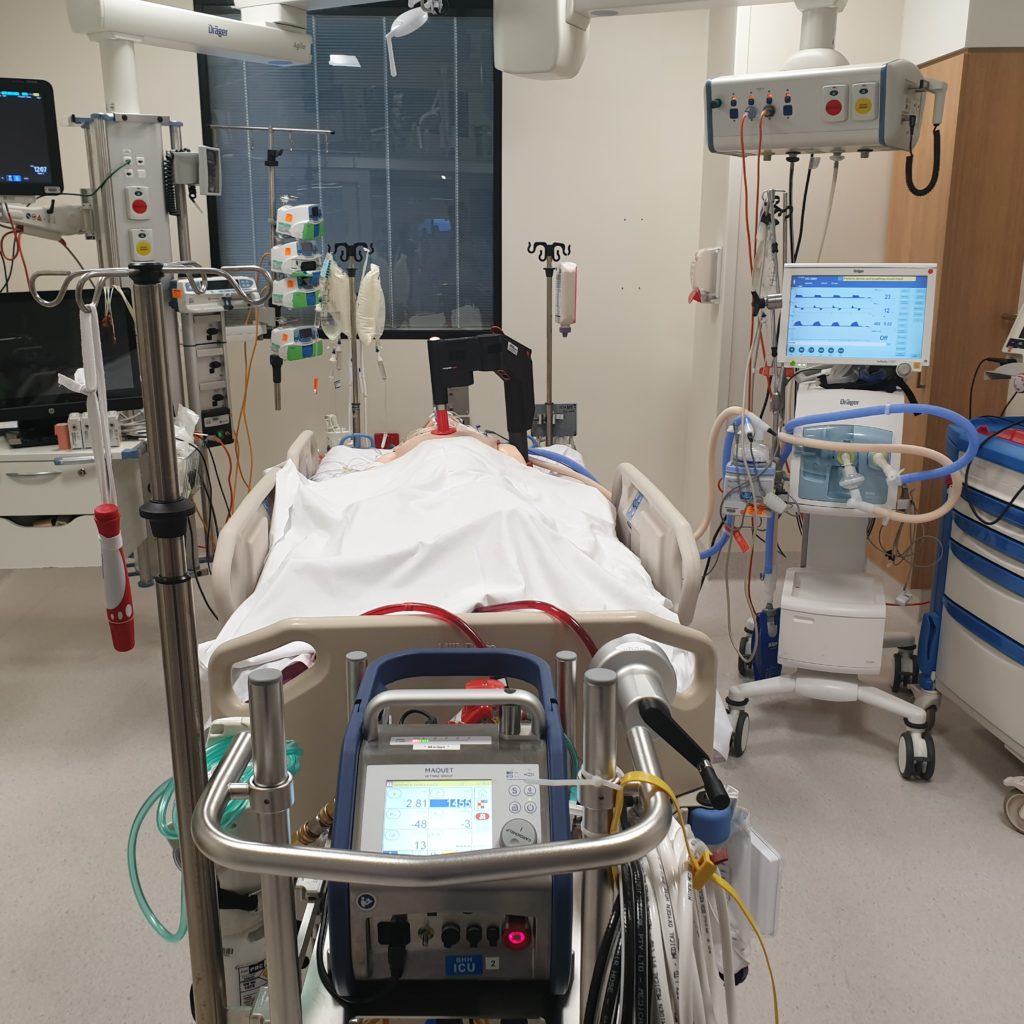
What ECMO does is that it drains venous blood from the right side of the heart, oxygenated it and returned oxygen-rich blood back to the patient. This process temporarily replaces the function of either the heart or lung and allows them to rest and recover. As ECMO supports your other vital organs, it provides the time needed by the medical team to address and fix the underlying problem.
Another advanced form of ECMO is ECMO-CPR (ECPR). Patients are pronounced dead in the field after 45 minutes of advance resuscitation if there is no return of circulation (ROSC). Now with ECPR service, patients with a refractory cardiac arrest can be supported by ECMO, maintaining cerebral and other vital organ perfusion while waiting for blocked coronaries to be stented in the Cath lab.
There is a free online resource provided by ELSO (peak organisation for ECMO) here: ECMO 101 | ELSO | Extracorporeal Membrane Oxygenation if you are keen to know more about ECMO.
What is a Critical Care Echocardiographer?
Critical care echocardiography is a sub-speciality branching from conventional echocardiography. As a critical care echocardiographer, I provide point-of-care cardiac ultrasound to answer time-critical questions within the ICU: why is the patient hypotensive? Is there evidence of cardiac tamponade or ischemia? Does the patient have PE? Is there a cardiac contributing factor to why patient cannot be weaned off the ventilator?
As an experienced critical care nurse with added echocardiography capability and qualifications, I am enabled with the ability to provide repeated cardiac ultrasound. This adds value to monitoring and evaluating the effectiveness of interventions for ECMO patients, it is immensely satisfying and professionally rewarding. This betterment of the patients’ outcome was my primary motivator when I undertook cardiac ultrasound training
How does someone become an ECMO nurse or cardiac sonographer?
As you would imagine that patients on ECMO are the sickest within the ICU population, ECMO nursing staff must be at least a Critical Care Registered Nurse (CCRN). This is because patients on ECMO are also likely to require other organ support systems. These could be medications to maintain circulation, haemodialysis to support renal function etc. Thus ECMO nursing brings together the skill-set and technological know-how of all these organ support systems.
In Victoria, an ECMO nurse needs to complete a 2 day ECMO course at a ELSO centre and also pass a series of own in-house theory and practical competencies to become a full-fledge ECMO competent nurse.
For a cardiac sonographer, you have to complete a 2-year traineeship alongside a 2-year university program (such as at QUT) recognised by Australian Sonographer Accredited Registered (ASAR).
What is your role as an ECMO coordinator?
Like our ED colleagues, I do not know how the day would turn out. You can be placing ECMO support electively in the Cath lab or ECPR in ED/ ward, however, a typical day consists of administrative and research work. Some of the other stuff I do behind the scene includes stock-take of equipment, education planning, rosters for on-call shifts, data coordination and lots of reading!
How has COVID19 impacted you and your ICU?
Nurses and nursing had shown so much resilience during the peak COVID19 outbreak in 2021. We have all come together during the time of need, regardless of our training/speciality (general RN/ theatre nurses etc) to care for some of the sickest COVID patients in the ICU. Some of these young patients (as young as 30s) are so unwell very quickly that conventional ventilation and its adjunction therapies were no longer able to support the patient through their disease process.
We administer paralysis and prone these patients to improve their oxygenation. When paralysis and proning fail, we will place suitable patients onto ECMO. These patients are the sickest of the sick. 2021 had placed unprecedented demand for ECMO due to COVID and also the fallout of dealing with a sicker patient population.
We have placed more than 23 patients onto ECMO. That is more than 2019 and 2020 combined together. We are very fortunate to work in an organisation that places a strong emphasis on ECMO training for nursing staff. We currently have more than 50% of our staff trained to prime an ECMO circuit, initiate ECMO and care for them. The collegial efforts have enabled the ECMO service to be provided 24/7, benefitting the communities living around us.
One reality of ICU nursing is that we don’t say NO! to admitting patients to the ICU because it isn’t our speciality. The ICU takes in all patients’ medical specialities that exist within the hospital. This adds to the complexity of ICU nursing offers.
Take for example disease progression in COVID patients, no one would have a good understanding of this before 2021. But together we learned and shared experiences to better these patients’ care. That’s the beauty of ICU nursing, we’ll keep finding solutions and continue to evolve to better the operational process and nursing practices.
What are some silver linings from the pandemic for nursing?
The COVID pandemic has brought a lot of attention to the state of critical care service and nursing. It’s great to have the state government recognise the infectious (occupational) hazards we face in our line of work during COVID19. I hope there will be continued recognition for nursing staff who continues to face such hazards in their line of work nationally (such as hyperbaric nursing, oncology nurses dealing with chemo/ radiation therapy etc.)
Also as I had mentioned earlier, COVID has brought a lot of nurses together to the ICU so there’s considerable up-skilling of the nursing workforce.
Advice for someone wanting to do something different.
I suspect that there will be more CCRNs in the future wanting to acquire a skill-set that is unique and highly valuable to their workplace (such as ultrasound, vascular access capability). It is challenging to complete this training, but not entirely impossible. You need to understand what is the nationally recognised credentialing for that skill-set, get your organisation to support you, and to incorporating these extra skill sets (whatever it be) into your scope of practice.
It is important to do your own research into the feasibility and sustainability of such endeavours to gain the support needed for such roles. Since these are likely to be senior positions, it is important to realise that the organisation would also want to ’test’ your ability to navigate certain challenges on your own during this endeavour. Keep knocking on doors and don’t give up!
Top 4 tips for a new nurse to ICU?
Ask your seniors for help. We want you to succeed.
Trust yourself. You got this.
There is no emergency in an infectious pandemic. Look after yourself 1st, PPE up properly and Go.
If we can bring the dead back alive (ECPR), anything is possible!
What’s next for your nursing career?
I will be pursuing my Masters of Nurse Practitioner at Monash University, hoping to bring all the skill sets altogether in a nurse/ nursing capacity.






You must be logged in to post a comment.