Table of Contents
We teamed up with Monash Health – Victoria’s largest public health service to interview one of their senior Neonatal Intensive Care Unit (NICU) Nurses about all things NICU nursing! Learn about what they do, the unique conditions they care for, the high-end equipment that supports them and so much more! A must-read article for all budding ICU, NICU and paediatric nurses.
Meet Josh!
Hi, I’m Josh and I am an Associate Nurse Manager in Victoria’s largest Neonatal Intensive Care Unit. I am in my fifth year of nursing with a previous background in ambulance and pre-hospital health. I have experience working in both Neonatal and Paediatric Intensive Care at two of Melbourne’s largest paediatric hospitals. I have also, until recently taught undergraduate nursing as an educator and lecturer.
I am currently studying epidemiology and disaster crisis medicine, an odd combination I know. My goal is to complete a doctorate degree exploring staffing models for best patient outcomes. Anyway, enough about me, let’s talk about the very specialised world of Neonatal Intensive Care!
What is a NICU nurse? And why do you love this speciality?
A Neonatal Intensive Care (NICU) nurse is a critical care Registered Nurse who provides care to unwell newborn infants who may have a variety of different problems ranging from prematurity to congenital defects, sepsis, and cardiac anomalies. A day in a life of a NICU nurse is rarely the same and will consist of caring for sick babies, attending high-risk deliveries and neonatal codes, as well as providing education and supporting new parents.
Neonatal nursing is very rewarding, yet in many respects challenging. For me, one of the most challenging aspects of my role is to watch the hopes and dreams of many families not turn out how they had hoped. To watch a family, make the decision to withdraw care on their baby, or to witness a sudden deterioration in which all care avenues have been exhausted is incredibly challenging.
Whilst supporting families through such an ordeal is incredibly rewarding, it will always bring some emotional challenges no matter how much experience one has in having to manage it. However, for every incidence of a poor outcome, there are so many positive and joyous stories.
We as neonatal nurses have the privilege of sharing so many joyous and momentous occasions with families, from the moments of the delivery of their baby, their first cuddle, their first bath, each and every milestone, and the day that they finally get to go home. Yes, as with any critical care specialty, we witness loss and grief, but we also see positivity and this makes our role so very rewarding.
What type of patients do you care for and what is your role in their care?
Conditions that we care for in the NICU are so broad and often very specific to the neonatal speciality.
Hydrops Fetalis
Hydrops Fetalis, or shortened to Hydrops, is a serious and life-threatening condition that we see in the NICU from time to time. The condition essentially occurs when fluid leaves the infants bloodstream and fills into the tissues. There are a number of potential causes, one cause is a haemolytic disease in which the baby is suffering from a complication of Rh incompatibility, in essence, the mother has an Rh-negative blood type whilst the baby has an Rh-positive blood type. The most common cause of this derives from the impairment of the body’s capability to manage fluid; such as heart and lung issues, severe anaemia (often from infections), or genetic abnormalities.
Unfortunately, complications of Hydrops can lead to fluid accumulation around the heart (pericardial effusion) and can lead to tamponade (fluid is putting pressure on the heart and preventing it from pumping effectively). Meanwhile, the fluid build-up in the lungs can make supporting the infant’s breathing status very difficult. Fluid can accumulate anywhere.
We manage the condition with mostly supportive measures, such as respiratory and airway management, inotropic support, as well as the use of drains to remove the accumulating fluid. Whilst I have no images of this condition to share (as you would expect), I recommend giving this condition a search on google images to get a more detailed understanding of what these poor babies go through.
Congenital Diaphragmatic Hernia (CDH)
Congenital Diaphragmatic Hernia is a congenital abnormality that occurs in-utero (in the uterus) at around 12 weeks gestation, in which the infant’s diaphragm, unfortunately, doesn’t form properly. This results in herniation of the baby’s abdominal contents, by consequence poor lung growth and development (pulmonary hypoplasia) occurs. This, along with abnormal pulmonary vascular development can cause pulmonary hypertension (higher pressure within the pulmonary arteries). Generally, the NICU medical and nursing outreach team will be in attendance at the delivery of a baby with known CDH (generally up to 85% of CDH are antenatally diagnosed), the team will intubate, manage cardiovascular issues, and immediately transfer the baby to the NICU for ongoing management and care. CDH is a complex condition to manage with a lot of consideration needed into their care. When the infant is stable, they will undergo a surgical repair, and this usually takes place within the NICU.
Necrotising Enterocolitis (NEC)
Necrotising Enterocolitis, which we call NEC due to our love of shortening everything, is a gastrointestinal condition that can often be very severe. It is more common in our premature infants (approximately 9 in 10) and occurs when intestinal tissue becomes inflamed and begins to die, causing the bowel to become ischemic and necrotic. This can then cause the baby’s bowel to perforate. Whilst not all NEC cases are severe, and if caught early, can sometimes be treated conservatively with “gut rest” where we make the baby ‘nil by mouth’ and managed with three different types of intravenous antibiotics for a few days, and monitor closely. However, in severe cases, NEC is a medical emergency that requires surgery to remove the diseased bowel. This can then cause significant infections, intestinal strictures (narrowing of the bowel), short gut syndrome (malabsorption due to shortening of the bowel), and developmental delays.
Hypoxic Ischaemic Encephalopathy (HIE)
Unfortunately, deliveries aren’t always straight forward, and on occasions deliveries that we don’t expect to be high-risk suddenly become so. On occasions, babies can be born in poor condition and require extensive resuscitation for a number of reasons, such as placental abruption, umbilical cord issues, or a significant bleed. When these things happen, the baby can experience a prolonged reduction or absence of blood flow to the brain.
This causes brain dysfunction, whilst most organs can often return to somewhat normal quite quickly after a period of ischemia, the brain doesn’t always recover quite like other organs. We call this Hypoxic Ischemic Encephalopathy (HIE). Babies may often present very floppy and what we call “hypotonic” which is when their tone is too relaxed, and sometimes “hypertonic” where they appear stiff. They may present with abnormal movements and seizure-like activity. Generally, once these babies have stabilised after resuscitation, they may require respiratory support, cardiovascular support, therapeutic cooling, and monitoring for electrical seizure activity.
Cooling occurs using a machine called the “arctic-sun,” we cool the babies on what is essentially a cool blanket to bring the baby’s temperature to a few degrees below their usual temperature, this will then hopefully reduce further brain injury. We will usually also monitor for seizure activity using a “brainz” monitor, this is an EEG monitor where we insert tiny needles into the baby’s scalp. This will give us a live trace of the baby’s brain activity. We will of course give the baby medications and infusions to keep them comfortable during this treatment. After three days of cooling, we then begin a process of very slowly rewarming the baby back to their regular temperature.
Chronic Lung Disease (CLD)
Chronic Lung Disease (CLD) generally refers to persistent respiratory issues in premature infants. Also called bronchopulmonary dysplasia, it can often be caused by needing prolonged oxygen therapy, pulmonary damage during mechanical ventilation, infections, or simply underdeveloped lungs due to prematurity. A common concern with any baby delivering prematurity is “how good are their lungs?”.
Whenever a baby is expected to deliver prematurely, the midwives on birth/delivery suite will administer steroids to the mother in order to accelerate the development of the baby’s lungs. However, this takes time, and sometimes time isn’t always on our side and as a result these steroids may not have time to take full effect.
On occasions, the requirement for the baby’s delivery may be more emergent, and there is no time for these steroids to be administered. Babies with these issues present with respiratory distress and often require prolonged respiratory support and oxygen. Many will be discharged home on some form of oxygen therapy.
Specialised NICU Equipment
Check out some of the specialised NICU equipment below!
SensorMedics
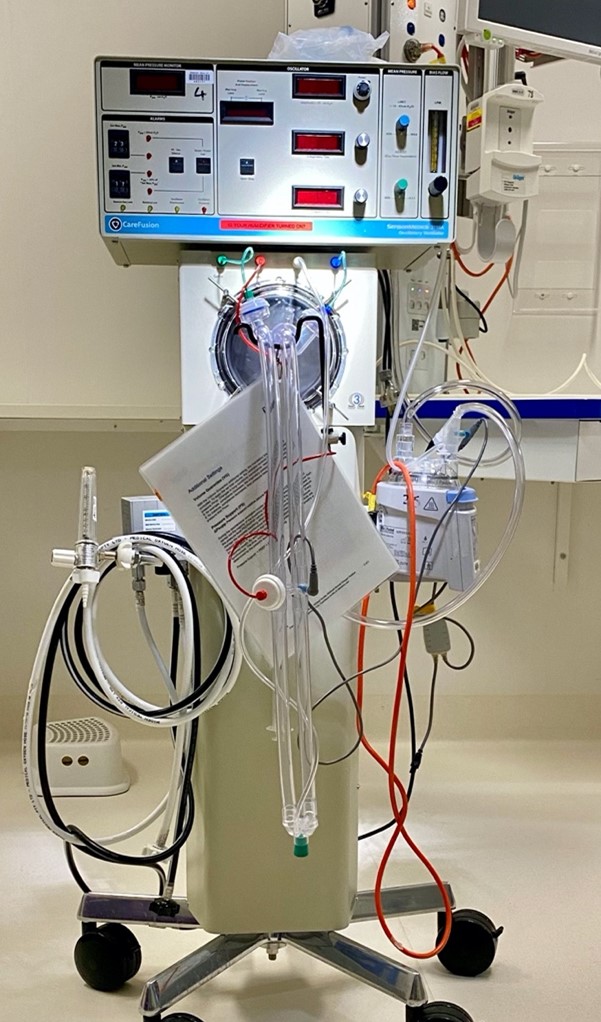
SensorMedics
The SensorMedics is a mechanical ventilator known as a High Frequency Oscillatory Ventilator (HFOV). This ventilator is essentially a drum. The use of SensorMedics allows us to maintain a more constant mean airway pressure (average pressure within the airway over time) and is utilised as a rescue therapy.
So, we utilise this when more conventional forms of ventilation aren’t giving us the result we were hoping for. With HFOV we “drum” air at high frequency. This ventilation rate is measured in cycles per second known as hertz. 10Hz is 10 cycles per second, resulting in 600 cycles per minute.
Nitric Oxide (iNO)

Nitric Oxide (iNO)
Nitric oxide is a gas that we connect to the baby’s ventilator. It works to relax smooth muscle thus dilating blood vessels. This is a localised vasodilator, so by inhalation we see this dilation occur in the lungs.
This helps in treating respiratory failure by reducing the pulmonary vascular pressures and allow blood to flow to the pulmonary vessels more effectively.
Arctic Sun

Arctic Sun
The Arctic Sun is the equipment used to therapeutically cool a baby as referenced above under HIE. This machine maintains the baby’s cooler core temperature with the use of its own core temperature measurements.
This allows for more consistent therapy. The machine will also time the length of time that the baby has been cooled and will automatically begin the rewarming process. The warming process is very gradual and managed by the Arctic Sun.
‘Brainz’ Monitoring
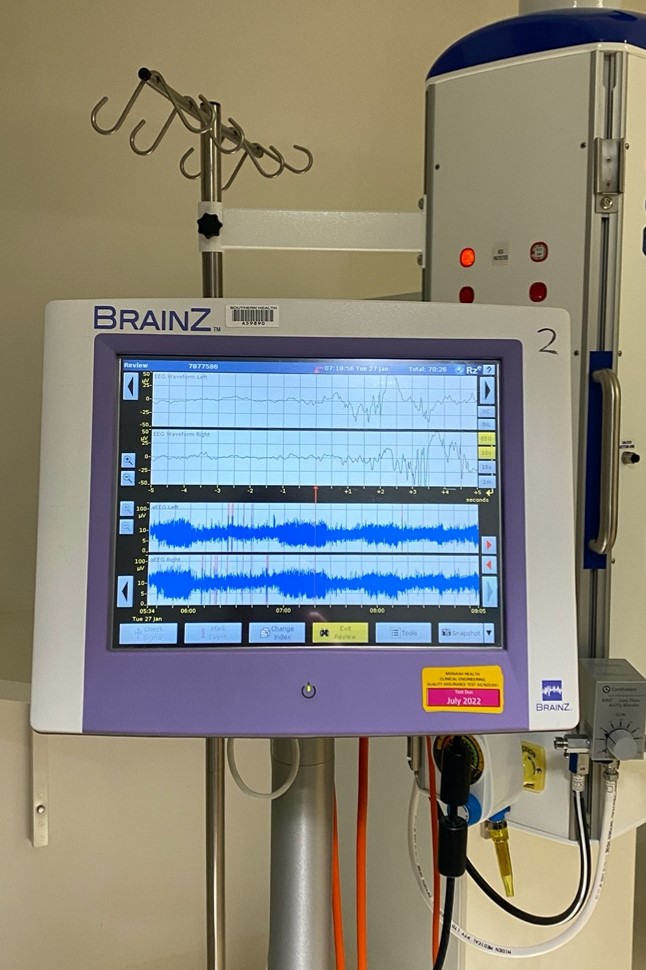
‘Brainz’ Monitoring
The ‘Brainz’ monitor is an ambulatory electroencephalography (aEEG), this allows us to monitor and record brain wave patterns picking up on potential seizure activity.
This monitor works by the insertion of four small needle probes placed just beneath the baby’s scalp. We then allow the monitor to record brain waves until we are satisfied with the diagnostic data.
Transport Cot

Transport Cot
The transport cot is basically what the name indicates. This cot allows for the safe transport of unwell neonates around the hospital, this could be from delivery, surgery, MRI etc.
The cot maintains a steady temperature to keep the baby warm. Other equipment, including a ventilator, resuscitator, monitor, and other emergency equipment/medications are carried on the cot.
What advice would you have for other health professionals in dealing with acutely unwell and dying children?
Everybody will have different coping mechanisms in dealing with this, I don’t think there is necessarily a right or a wrong way. As nurses we have a lot of empathy, we work closely with families and parents for long periods of time, and to hear their cries after their baby has passed is a lasting experience. It is something that I have never been able to get used to, every incidence is as traumatic as any.
As a human being it is difficult to wrap your head around a baby or child dying, it doesn’t seem fair or the natural order of things. I often wonder if we’re doing the right thing when the decision to withdraw care is made. Is there anything more we could do? What if we have missed something?
Then on the other hand, the child is on every haemodynamic support we have, inotropic support just to maintain a bare minimum mean arterial pressure. The significant morbidity and poor quality of life should we manage to miraculously save their life. There are a lot of conflicting thoughts and feelings during the process.
“I believe that debriefing is a really important part of losing a patient, both informally and formally”.
I believe that debriefing is a really important part of losing a patient, both informally and formally. It is important to talk, to discuss what learnings we can take from the situation, whilst taking a moment to reflect on what we all have experienced. I feel it’s important to have some form of offload before you leave your shift. Of course, you will continue to reflect, many may cry in the car on their way home, we’re only human. Many will say alcohol isn’t a healthy option in this instance, I say stuff them, if you want a glass of wine, have a glass of wine! (drink responsibly etc)
How do you become a NICU nurse?
Apply! I would say on average neonatal units will advertise once or twice a year. Usually, one year of acute nursing experience is needed, so as soon as you’ve completed your graduate program! You will be expected to study within a certain amount of time, a graduate certificate is usually the minimum
As with all specialities, neonatal nursing is very safety focused! Being proactive with patient safety, as well as your own professional development and learning is always very well received!
See more paediatric/neonatal related articles here or ICU related ones here





You must be logged in to post a comment.