Author: Gisele Guenard, BScN, MEd, VisionarEase Inc. & associates CEO, Founder – Client Centered Governance ® Essentials Certification & Nonprofit strategic planning services. @GGVisionarEase
Warehouses for Death – Decades ago, research I completed for an undergrad paper drove me to pen ‘Warehouses for Death’ as its title. Accountability and risk management were not part of the paper’s lexicon: it was more of a whistleblower-styled piece. I was a post-RN student in the BScN program at Laurentian University in Sudbury, Ontario. This was in the 80s, before Long-Term Care (LTC) Standards were anywhere near what they are now. It was common then, and I’m afraid still today, to hear seniors swear they would never “go into a nursing home, because that’s where people go to die.” Topping the list of answers to the question, “How did we get here?”, is the fact that LTC was never protected as other areas were, when our health care system was cobbled together in the ’60s, nor when the Canada Health Act became law in the ’80s.[1] I do know however, that excellent care is being provided in many LTC homes, most of the time. It is those times when systems can fail, such as a pandemic, that have brought the current crisis in LTC. And we can change that.
 The COVID-19 Pandemic has tragically revealed that safety and the quality of care in many LTC homes remains far from where it needs to be. Leaders across the sector have loudly echoed the calls for change seen in media since March 2020 – when the World Health Organization (WHO) declared a global pandemic. This call from leaders includes Ontario’s scathing Long-Term Care COVID-19 Commission Interim report.[1] The Canadian Institute for Health Information (CIHI), revealed in 2020, that Canada’s dismal record on COVID-19 mortality included this statistic: over 80% of 1st-Wave deaths were in LTC. This was a powerful call to action: our death rate was twice the international Organisation for Economic Co-operation and Development (OECD) average.[2]
The COVID-19 Pandemic has tragically revealed that safety and the quality of care in many LTC homes remains far from where it needs to be. Leaders across the sector have loudly echoed the calls for change seen in media since March 2020 – when the World Health Organization (WHO) declared a global pandemic. This call from leaders includes Ontario’s scathing Long-Term Care COVID-19 Commission Interim report.[1] The Canadian Institute for Health Information (CIHI), revealed in 2020, that Canada’s dismal record on COVID-19 mortality included this statistic: over 80% of 1st-Wave deaths were in LTC. This was a powerful call to action: our death rate was twice the international Organisation for Economic Co-operation and Development (OECD) average.[2]
At the time of writing Warehouses for Death, I had done placements in ‘nursing homes’ and ‘old age’ homes, as they were termed then, and worked as an RN on Long-Term and Continuing Care hospital units, always hoping for the “we gave excellent care” feeling, when our teams reported off at shift change. Add to that, what I had seen in the LTC units of the massive psychiatric hospital I had worked in as a student in the 70s. Those memories have never left me. All of what was most disturbing for residents of LTC, would have been a non-issue, had effective governance, leadership, as well as care Standards of accountability and risk management been in place at all levels.
Today in 2023, the challenge persists for LTC facilities to meet current and new Standards with existing funding, provincial/territorial-federal funding disputes, and the puzzle of various, inconsistent, toothless LTC Standards in multiple jurisdictions. Boards and leadership teams of LTC facilities are to be commended for the successes they have achieved, as the situation is not all dire, all the time. Nurses and all members of LTC care teams are performing difficult, exhausting work with our most vulnerable, often with inadequate resources. We work with LTC Board and leadership teams and have seen excellent, ‘beyond the call of duty’ care, over and over. They all care deeply for the residents who depend on their vigilance and expertise.
However, as a society, we have scored poorly in our overall creation, maintenance, funding and oversight of Long-Term Care in Canada, the most disturbing element being the staffing crisis. Beverly Mathers, then-CEO of the Ontario Nurses Association, was quoted in the Ontario Long-Term Care COVID-19 Commission’s letter to then Minister of LTC, Dr. Merrilee Fullerton:
“So since at least 2001, numerous reports have been written confirming what staff who work in long-term care have known, that long-term care is grossly inadequate, their staffing, and given the acuity and care needs of the residents which has grown year over year.”[4]
We need effective, evidence-based common Canadian LTC Standards, with the required funding for implementation.
(LTC 2023 How did we get here? See full size graphic at the end of the blog)
Accountability & Risk Management: it’s about Leadership in Safety & Quality Care – From the governing bodies of LTC facilities, to their leadership teams and front-line care providers, where accountability and risk management are poor, LTC residents suffer from safety gaps and inadequate quality of care. Where the opposite is true, resident outcomes are better and the appreciation from families is notable, while recruitment and retention are much less of a challenge than in other facilities.
Accountability and risk management are the twin engines of positive Client outcomes for healthcare facilities. And the Board of Directors[4] is piloting that plane. Experience with amazing governance teams has taught me that today, for many nonprofit LTC facilities, the Board of Directors [5] is highly engaged and intent on resident safety, quality care, risk management and accountability. However, unless safety and quality drivers such as LTC Standards are closely adhered-to and outcome accountability present, risk management practices will fail.
 Research confirms that accountability and risk management practices, when Board-led, Client-centered and embedded in the very culture of health care organisations, contribute to the prevention of errors, and save lives.[6] Where this is weak, catastrophic failure is too often the reality. It was not so long ago, that hospitals and LTC facilities commonly operated without safety and quality improvement systems in place. No tracking of indicators. No public reporting. The 1980s saw a major shift in LTC, with governments raising the bar from their long-standing ‘hands-off’ stance, to begin setting policy through legislation, to drive positive change towards better quality of life for people, mostly seniors, who were ‘nursing home’ residents.
Research confirms that accountability and risk management practices, when Board-led, Client-centered and embedded in the very culture of health care organisations, contribute to the prevention of errors, and save lives.[6] Where this is weak, catastrophic failure is too often the reality. It was not so long ago, that hospitals and LTC facilities commonly operated without safety and quality improvement systems in place. No tracking of indicators. No public reporting. The 1980s saw a major shift in LTC, with governments raising the bar from their long-standing ‘hands-off’ stance, to begin setting policy through legislation, to drive positive change towards better quality of life for people, mostly seniors, who were ‘nursing home’ residents.
Boards and Executive leaders were required to step up accountability and risk management strategies to meet new, clear and stringent Standards. Inspections were common, unannounced, and carried compliance infraction notices with timelines when required. In Ontario, health care facilities in the hospital, LTC, as well as mental health and addiction sectors, are now required to have a publicly posted Quality Improvement Plan (QIP) in place, and to submit data to Health Quality Ontario (HQO). Will the launch Canada’s new Long-Term Care Standards be the watershed moment Canadian LTC residents and families need to take us to the next level? Without attached compliance requirements, possibly tied to transfer payments, it will be up to the provinces and territories to make changes within their own jurisdictions – a highly politicized issue.
Leaders of LTC must govern and operate with complex factors including an aging population cohort with an increasing incidence of chronic conditions, the latest tech and new, expensive drugs, all contributing to rising health care costs. Compounding the areas of risk and related accountability requirements, are the number of Adverse Events (AEs) occurring… disturbingly high. So high, were certain AEs in LTC, that tracking of these in QIP reports now includes for example, indicator data for the number of LTC residents receiving antipsychotics without a related diagnosis, and the number of instances of restraint use. Both indicators are red flags for potential AEs.[7] And many LTC facilities are succeeding in improving safety and care in these areas, through evidence-based care strategies.[8]
A constantly changing array of statutes and regulations applies to LTC, and governing teams must ensure compliance, regardless of the challenges. In Ontario for example the new “Fixing Long-Term Care Act” and its Regulations were enacted in the fall of 2022, triggering a massive re-evaluation of practices and related modifications.[9] Change is constant and LTC is not immune: governance teams must apply the same accountability and risk management practices to all these challenging issues
 A Brighter Day for Long-Term Care Residents – Ontario has comprehensive, stringent, legislated LTC requirements and Best Practice Standards from various sources. LTC homes are striving to comply with these and even go beyond them, making positive changes wherever possible. This includes evidence-based dementia care, providing more primary care with the inclusion of Nurse Practitioners, installing air conditioning, physiotherapy on site and more.
A Brighter Day for Long-Term Care Residents – Ontario has comprehensive, stringent, legislated LTC requirements and Best Practice Standards from various sources. LTC homes are striving to comply with these and even go beyond them, making positive changes wherever possible. This includes evidence-based dementia care, providing more primary care with the inclusion of Nurse Practitioners, installing air conditioning, physiotherapy on site and more.
Added to the positive change and advocacy movement, the voices of Ontarians have joined in the decades-long plea to increase the legislated Standard for hours of resident care per day. This call has been heard by the provincial government. New legislation, the “Fixing Long-Term Care Act”, requires LTC facilities to scale up to four/4 hours per resident per day by March 2025, from the current 2 hours and 45 minutes.[10] The increase in required care hours will be a challenge to implement in many LTC facilities, largely due to gaps in the availability of care providers and inadequate funding.[11] The statute outlines a timeline of yearly targets, which will no doubt require additional funding and governance oversight to ensure compliance.
Available Best Practice Standards include those developed by Health Quality Ontario (HQO), which include detailed tools and resources, all at no charge, whereas other Standard-setting bodies may charge for access.[12] HQO has published Best Practice Standards for fourteen common health conditions, with easy-to-follow guidelines for facilities to work with, including evidence-based indicators.
Accountability and risk management require that governance teams be familiar with the Standards their LTC home is required to meet. The Board, for example, must receive regular data on measurement and monitoring of key indicators. For example, one of HQO’s Best Practice Standards addresses ‘Diabetic Foot Ulcers’, with several indicators which could be tracked, such as ‘Percentage of patients with a diabetic foot ulcer who had lower extremity amputation in a six-month period’.
 Ontarians will see the building and creation of 30,000 new LTC beds by 2028. This commitment is long overdue and is a monumental project to be tackled by LTC Boards, Executives, facility owners and their partners. However, for every community slated to receive additional LTC beds, this is welcome news.[13] Additionally, 30 LTC projects to serve Indigenous communities, and 39 projects for the Francophone population have been announced. Health Human Resources (HHR) needs will be great, and must be addressed by political leadership, funding, and collaborations between academic and LTC provider agencies.
Ontarians will see the building and creation of 30,000 new LTC beds by 2028. This commitment is long overdue and is a monumental project to be tackled by LTC Boards, Executives, facility owners and their partners. However, for every community slated to receive additional LTC beds, this is welcome news.[13] Additionally, 30 LTC projects to serve Indigenous communities, and 39 projects for the Francophone population have been announced. Health Human Resources (HHR) needs will be great, and must be addressed by political leadership, funding, and collaborations between academic and LTC provider agencies.
Organizations and individuals have long been calling for positive change to federal > provincial funding for health care, including LTC. Included in this advocacy were regulated health professional associations such as the Canadian Nurses Association (CNA). This advocacy has contributed to the Canadian government recently reaching an agreement with the provinces and territories, to increase health care investments intended to deliver better outcomes for patients and communities. In a press release days before the federal announcement, Sylvain Brousseau, president of the CNA stated:
“We are pleased to see proposed federal investment in key areas of concern for nurses and health-care workers across Canada, and recognize this as a first step in addressing the gaps in the health-care system.” [14]
and Tim Guest, CEO of CNA:
“Nurses across Canada are in need of support and resources to address the critical shortages and gaps in service. CNA urges all governments to move quickly to finalize bilateral agreements, with key indicators for creating a sustainable health-care workforce”.
 Part of the federal investment announced Feb 23, 2023, is slated to address the HHR crisis, with nursing and personal support worker shortages being the most critical of gaps for LTC. $198.6 billion is to flow over 10 years. This includes $46.2 billion with new immediate unconditional funding of $2 billion as a Canada Health Transfer (CHT) top-up, to address “immediate pressures on the health care system”.[15] Within its goals, the overall funding is intended to bolster a struggling HHR sector, and create a “resilient and supported health workforce that provides them high-quality, effective, and safe health care services”.[16] Will this have a trickle-down impact for HHR in LTC? LTC residents, families, Boards and staff certainly hope so. The funding also includes $1.7 billion over 5 years, “…to support hourly wage increases for personal support workers and related professions, as well as through the joint investment with provinces and territories of $6 billion over 5 years for home and community care.”[17] Increasing the number of Registered Nurses on site, and Nurse Practitioners providing comprehensive primary health care in LTC homes, must be part of these initiatives.
Part of the federal investment announced Feb 23, 2023, is slated to address the HHR crisis, with nursing and personal support worker shortages being the most critical of gaps for LTC. $198.6 billion is to flow over 10 years. This includes $46.2 billion with new immediate unconditional funding of $2 billion as a Canada Health Transfer (CHT) top-up, to address “immediate pressures on the health care system”.[15] Within its goals, the overall funding is intended to bolster a struggling HHR sector, and create a “resilient and supported health workforce that provides them high-quality, effective, and safe health care services”.[16] Will this have a trickle-down impact for HHR in LTC? LTC residents, families, Boards and staff certainly hope so. The funding also includes $1.7 billion over 5 years, “…to support hourly wage increases for personal support workers and related professions, as well as through the joint investment with provinces and territories of $6 billion over 5 years for home and community care.”[17] Increasing the number of Registered Nurses on site, and Nurse Practitioners providing comprehensive primary health care in LTC homes, must be part of these initiatives.
At the federal level in 2020, through Canada’s new Long-Term Care Standards release, the Canadian government has made improving Long-Term Care across Canada a mission. 19,000 Canadians participated in informing the new Standards. So far, three leading organizations have collaborated to develop two detailed new Standards that pertain to health care and community organizations, including LTC:
- The Standards Council of Canada (SCC)[18]
- The Canadian Standards Association (CSA Group)[19] . Focus: design, operation, and infection prevention and control (IPAC) practices
- The Health Standards Organization (HSO)[20]. Focus: delivery of safe, reliable, and high-quality long-term care services
Two new voluntary LTC Standards have been released by the Canadian government. These detailed, comprehensive Standards were developed through a rigorous process, a massive endeavour which included the following steps:
- Identify – Identify opportunities for Standard review
- Study – Preliminary study in preparation of a draft outline
- Public review – Public review of the draft outline
- Publish – Publish the Standard
- Committee – Finalize project proposal and establish technical committee
- Consensus – Committee meetings and consensus building on the draft
- Approve – Vote on the draft Standard.[21]
- CAN/HSO 21001:2023 (E) Long-Term Care Services / Please follow the reference link for in-depth details.[22]
 “The Standard focuses on promoting good governance; upholding resident-centred care and enabling a meaningful quality of life for residents; ensuring high-quality and safe care; fostering a healthy and competent workforce; and promoting a culture of quality improvement and learning across long-term care (LTC) homes. The target audiences for the use of this Standard include LTC home residents, substitute decision makers, essential care partners, the workforce, leaders, and governing bodies. The content of this Standard is structured into the following sections:
“The Standard focuses on promoting good governance; upholding resident-centred care and enabling a meaningful quality of life for residents; ensuring high-quality and safe care; fostering a healthy and competent workforce; and promoting a culture of quality improvement and learning across long-term care (LTC) homes. The target audiences for the use of this Standard include LTC home residents, substitute decision makers, essential care partners, the workforce, leaders, and governing bodies. The content of this Standard is structured into the following sections:
- Governing LTC Home’s Strategies, Activities, and Outcomes
- Upholding Resident-Centred Care
- Enabling a Meaningful Quality of Life for Residents
- Ensuring High-Quality and Safe Care
- Enabling a Healthy and Competent Workforce
- Promoting Quality Improvement.
Accountability and Risk Management: included in this Standard, is guidance for LTC governing bodies to ensure:
- upholding strong governance practices and a culture that is outcome-focused and committed to continuous learning and quality improvement.
- CSA Z8004, Long-term care home operations and infection prevention and control
“This Standard provides guidance on safe operating practices, design, and IPAC in LTCHs while incorporating a person-centred approach. The Standard takes into consideration what is required during both normal, day-to-day circumstances and catastrophic events (e.g., outbreaks, epidemics, pandemics, fires, earthquakes, loss of power). The Standard considers factors such as homes of different sizes, resident acuity and demographics, and new builds vs. existing LTCHs.’[23]
It remains to be seen how and to what extent provinces and territories will comply with the new Canadian Standards and what the timelines will be for the safety and quality of care improvements to be implemented. It is probable that many LTC homes are, most of the time, already meeting these Standards, or well on their way to do so. With adequate funding and HHR, the outcomes will be excellent.
 Tools and Partners for Positive Change – One of the most important areas where new Standards are reflected are in accreditation programs, with governance Standards raising leaders’ accountability and risk management requirements:
Tools and Partners for Positive Change – One of the most important areas where new Standards are reflected are in accreditation programs, with governance Standards raising leaders’ accountability and risk management requirements:
“Standards create a strong health care structure that the public, providers, and policy makers can rely on, assuring high quality health services where it matters most.”[24]
Health Standards Org: CAN/HSO 1001:2022 – Governance
LTC Accreditation practices and tools have evolved into rigorous compliance initiatives, with organizations experiencing great pride in successful reviews and accreditation awards. Accreditation Canada is the leader in the sector for LTC, with its Qmentum Long-Term Care Accreditation Program:
“Accreditation Canada’s Qmentum Long-Term Care accreditation program helps providers meet global Standards, putting mechanisms in place that lead to safe and effective care. Our program will support building a culture of continuous quality improvement in long‐term care homes using clear language that is easily understood by residents, families, caregivers, front‐line staff and management.”[25]
LTC Boards can also improve their ability to govern through use of data and tools provided by LTC groups such as the Ontario Long-Term Care Association (OLTC). Deeper knowledge about LTC issues supports a Board’s ability to succeed in accountability and risk management. The OLTCA states its intent in keeping with resident-centeredness, accountability and risk management, safety and quality care:
“For 60 years, the Association has been committed to advancing the quality of long-term care services in Ontario. With advocacy and leadership as a key focus, the Association has been able to influence legislative, policy and regulatory change, support sector expansion and redevelopment, and provide educational opportunities to ensure the increasing needs of residents are being met with safe, high-quality care.”[26]
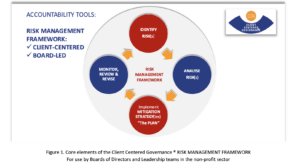
To be effective, risk management plans must be Resident-Centered and Board-Led. The CEO and staff team usually develops the documentation and collaborates with the Board to finalize. The core elements must include Risk Identification, Analysis, Mitigation and the Prevention of risk. The following ‘snapshot’ accountability tool is of value for Boards and all levels of operations within a LTC facility.
It, or a similar tool, should be part of orientation for Board members and staff in all LTC departments.[1] The related development of the comprehensive Risk Management Plan with effective measurement and monitoring of indicators becomes day-to-day tool for safety and quality care.
Conclusion – Canadians’ lifespan is increasing. Our senior years can be challenging, or we can experience more health, well-being and satisfaction than at anytime in history. When we face health conditions, sometimes complex and chronic, we need the support of a health care system that is operating from evidence-based Best Practices and Standards. We need to trust in this system, and to be confident that the right care will be there for us and our loved ones when we need it.
We may need the coordinated services of multiple care providers. We also need access to a LTC bed when we can no longer safely live in the community. It is not realistic to plan as if all Canadians will live in their own home until death. LTC homes that are effectively funded, governed, led and staffed, can provide positive outcomes for residents and families. Canadian and regional Standards, when mandated, can ensure safer, dependable quality services.
No more warehouses for death, and instead – Comfortable Safe Homes for Living Well. It is my hope and vision that Canadian and regional LTC Standards are evolving towards the best possible, sustainable framework for Canada’s most vulnerable adults. We can do this.
Thank you for your interest in Governance, Leadership, LTC Standards, Accountability & Risk Management.
Gisele Guenard
[1] https://laws-lois.justice.gc.ca/eng/acts/c-6/page-1.html
[2] http://www.ltccommission-commissionsld.ca/ir/pdf/20201023_First_Interim_Letter_English.pdf / COVID-19 Commission Final Report
[4] http://www.ltccommission-commissionsld.ca/ir/pdf/20201023_First_Interim_Letter_English.pdf Note: this reference has been archived. The URL is not live, and a copy and paste is required.
[5] The term “Board” is used in this document to indicate a Board of Directors, Board of Management, Committee of Management or other governing body of the LTC facility.
[6] RECOMMENDED (3): 1. Institute of Medicine (US) Committee on Quality of Health Care in America. TO ERR IS HUMAN: Building a Safer Health System. https://www.ncbi.nlm.nih.gov/books/NBK225170/#ddd00064 , 2. https://www.patientsafetyinstitute.ca/en/toolsResources/Canadian-Quality-and-Patient-Safety-Framework-for-Health-and-Social-Services/Documents/CPSI-10001-CQPS-Framework-English_FA_Online.pdf
and 3. https://www.healthcareexcellence.ca/en/resources/healthcare-quarterly/
[7] Examples of System Performance Indicator tracking/Ontario: https://www.hqontario.ca/System-Performance/Long-Term-Care-Home-Performance
[8] https://www.ismp-canada.org/download/AdverseEventsInLTC.pdf and see Sudbury’s Finlandia Hoivakoti Nursing Home Limited, with 0% Restraint use https://www.hqontario.ca/System-Performance/Long-Term-Care-Home-Performance/Long-Term-Care-Home-Performance/Wait-Times
[9] https://www.ontario.ca/laws/statute/21f39
[10] https://www.ontario.ca/laws/statute/21f39#BK15
[11] https://www.ontario.ca/page/long-term-care-staffing-study
[12] https://www.hqontario.ca/
[16] ibid
[20] https://longtermcareStandards.ca/
[21] https://longtermcareStandards.ca/about-Standard
[22] https://healthStandards.org/Standard/long-term-care-services-can-hso21001-2023-e/
[23] https://www.csagroup.org/store/product/CSA%20Z8004%3A22%20CANADA/ Note: you will need to create a free account to view the full Standard.
[24] https://healthStandards.org/Standard/governance-3/
[25] https://accreditation.ca/qmentum-ltc-accreditation/
[1] From professional development module/CLIENT CENTERED GOVERNANCE ® Essentials Certificate Course for Nonprofit Boards & Staff / About Client Centered Governance (R) Board Education Non Profit