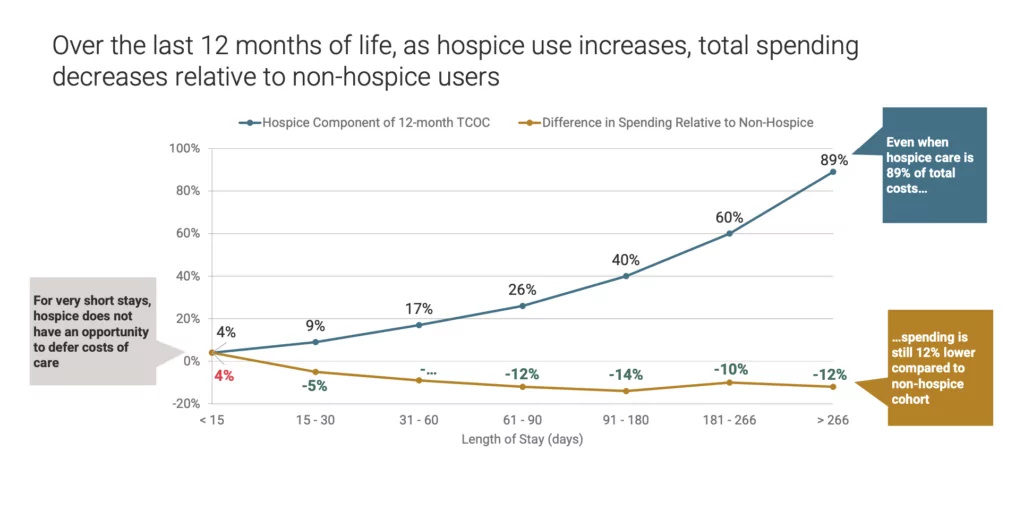
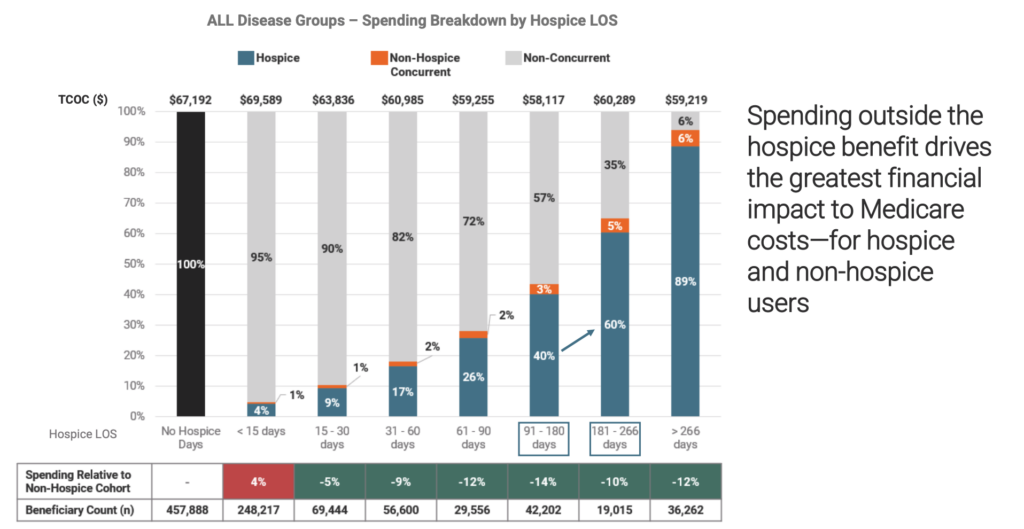
Despite years of scrutiny over the duration of hospice care, new data show that longer stays reduce health care costs in the last year of life by as much as 11%.
All told, hospice care — regardless of length of stay — saves Medicare approximately $3.5 billion for patients in their last year of life, a 3.1% reduction. But those with stays of six months or more yielded the highest percentage of savings.
A trio of organizations published these findings Wednesday in a joint report, including the National Hospice and Palliative Care Organization (NHPCO), the National Association for Home Care & Hospice (NAHC), and NORC at the University of Chicago.
“Hospice demonstrates improved quality of life, especially when people receive it over several weeks and months versus days, and is at the same time a better financial use of our resources,” NHPCO COO and interim CEO Ben Marcantonio told Hospice News. “That’s now supported in a very clear way. Responsible and clinically appropriate care for people with serious illness doesn’t always fit into that defined [six-month] length of stay that one might expect.”
Questions around appropriate lengths of stay have emerged as a contentious issue. Regulators generally consider stays that go beyond six months to be red flags, including the U.S. Centers for Medicare & Medicaid Services (CMS) and the U.S. Department of Health & Human Services Office of the Inspector General (HHS-OIG).
Case in point, OIG plans to conduct a national audit of hospice eligibility this year in which length of stay will be a key factor.
The issue received widespread public attention following a New Yorker/ProPublica article on hospice fraud, to which Hospice News responded in an editorial.
At the crux of the debate is the six-month terminal prognosis requirement, which some have called into question as diagnoses like dementia-related illnesses become more prevalent. Such conditions have unpredictable trajectories, making estimates of life expectancy even more complex.
The data suggest that shorter lengths of stay may be the bigger problem when it comes to spending, according to NAHC President Bill Dombi.
“The study itself really demonstrates that the focus should be much more on the short length of stays and what could be done to improve an earlier election in hospice, rather than focusing in with a presumption that long lengths of stay are inherently abusive or fraudulent,” Dombi told Hospice News. “There should be a willingness to take a look at the longer length of stays as potentially bringing this positive value to both the patient and to the Medicare program, to step away from the prejudice against long stays.”
In other findings, the report also indicated that the costs of hospice care “break-even” with care settings on Day 10 and begin generating savings on Day 11.
When sorted by diagnosis, cost reductions ranged from 4% lower for neurodegenerative illnesses to 25% for chronic kidney disease/end-stage renal disease, the report indicated.
But regardless of disease, spending in the last year of life is consistently lower for patients with stays of 15 days or more.
“Our research shows that hospice is an essential component of end-of-life care and should be prioritized in any attempts to secure the future of Medicare solvency,” Dianne Munevar, vice president of health care strategy at NORC, said in a statement. “For patients and families, our research provides one more reason to have conversations about end-of-life care before it is needed and to seriously consider hospice so that when the time comes their wishes and preferences are respected.”
A CMS spokesperson told Hospice News that the agency does on comment on data from outside entities. OIG also had no comment.
Companies featured in this article:
National Association for Home Care and Hospice, National Hospice and Palliative Care Organization, NORC at the University of Chicago